2025 July 27;6(7):929-937. doi: 10.37871/jbres2147.
The Veterans Affairs Lipid Optimization Reimagined - Quality Improvement Program: Rationale and Methods
Abigail A Santos1*, Jennifer DelGrande1, Abigail Fink1, Juhi Seth1, Courtney Bonnema1, Rachel Ward1, Helen M Wellman1, Nedim Yel1, Mason Coleman-Lopez1, Dakotah Feil1, Sharon Sharnprapai1, Kristin Colson2, Eddie Pan2, Tharen Leesch2, David Peña2, Michelle Congdon2, Michele Bolles2, Luc Djoussé1 and John Michael Gaziano1
2American Heart Association, USA
- Atherosclerotic cardiovascular disease
- Health coaching
- Cardiovascular disease
- Low-density lipoprotein cholesterol
- Dyslipidemia
- Quality improvement
- Veterans health
Abstract
Background: Atherosclerotic cardiovascular disease (ASCVD) is a major contributor to morbidity and mortality in United States (US) Veterans and to healthcare costs in the United States Veterans Affairs (VA) Healthcare System. Optimizing Low-Density Lipoprotein Cholesterol (LDL-C) can improve Veteran health, reduce incidence of cardiovascular events and death, and lower healthcare costs.
Methods: The VA Lipid Optimization Reimagined - Quality Improvement (VALOR-QI) program is an innovative three-year multi-site quality improvement program leveraging various lipid optimization strategies tailored to unique barriers and needs at 50 VA Medical Centers. Program oversight is provided by the Boston VA Coordinating Center and the American Heart Association (AHA), and local teams include a site lead or Clinical Champion (CC), a Healthcare Coach (HC), and a Health Care Provider Network (HCPN) of clinicians treating Veterans with ASCVD. Outcome data are collected through the VA electronic health record database and QI data are collected through the VA Research Electronic Data Capture (REDCap) system. Primary and secondary outcomes include the percentage of Veterans with optimized LDL-C (<70 mg/dL), absolute and percent change in LDL-C, use of lipid lowering therapies, medication adherence, cardiovascular risk score, and healthcare utilization and costs. Lipid optimization outcomes will be stratified by key Veteran demographics including geographic region, age, sex assigned at birth, race, and ethnicity.
Results: N/A- Program still in progress.
Conclusions: We will assess whether a novel quality improvement program can optimize lipids in Veterans with ASCVD at high risk for cardiovascular events, with subsequent improvement of Veterans’ health and reduction of costs for US Veterans and the VA Healthcare System. Findings from this program can inform clinical processes and guidelines for the VA Healthcare System and other healthcare systems alike.
Abbreviations
ACC: American College of Cardiology; AHA: American Heart Association; ASCVD: Atherosclerotic Cardiovascular Disease; BCC: VA Boston Coordinating Center; CC(s): Clinical Champion(s); CDW: VA Corporate Data Warehouse; CV: Cardiovascular; DoD: Department of Defense; HC(s): Healthcare Coach(es); HCP(s): Healthcare Providers(s); HCPN: Health Care Provider Network; LDL-C: Low Density Lipoprotein Cholesterol; LLT(s): Lipid Lowering Therapy(ies); Non-HDL-C: Non- High-Density Lipoprotein Cholesterol; NPC: Non- Profit Corporation; PHI: Protected Health Information; PII: Personally Identifiable Information; QI: Quality Improvement; REDCap: Research Electronic Data Capture; US: United States; VA: United States Department of Veterans Affairs; VALOR-QI: Veterans Affairs Lipid Optimization Reimagined - Quality Improvement Program; VAMC: Veterans Affairs Medical Center
What is Known
- Atherosclerotic cardiovascular disease is a leading cause of morbidity and mortality among United States Veterans and management of cholesterol is an effective way to prevent incident cardiovascular events in high-risk Veterans.
- A substantial proportion of Veterans with a history of stroke, myocardial infarction, and/or peripheral artery disease in the VA Healthcare System have LDL-C above target values, which can be attributed to personal, clinical, and institutional factors.
- Quality improvement programs are deployed in the VA Healthcare system to encourage system-wide and sustainable changes by identifying barriers to care, developing and implementing solutions, and integrating clinical and operational process improvements.
What this Study Adds
- We describe the unique structure and design of an ongoing novel quality improvement program carried out in collaboration with the American Heart Association that aims to improve Veteran cardiovascular health by addressing barriers to lipid management.
- Results of this program will offer insights into innovative avenues for optimizing lipids, reducing cardiovascular event risk, and improving overall cardiovascular health in a model that may be generalizable across other healthcare systems.
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is a major contributor to morbidity and mortality in United States (US) Veterans and to healthcare costs in the US Veterans Affairs (VA) Healthcare System [1,2]. Low-Density Lipoprotein Cholesterol (LDL-C) is an established major risk factor for cardiovascular events and management of LDL-C is an effective prevention measure for cardiovascular (CV) events in high-risk individuals, including those with ASCVD [3,4]. Despite the availability of effective Lipid Lowering Therapies (LLTs), approximately two thirds of Veterans with ASCVD in the VA have elevated or suboptimal LDL-C (defined in this program as LDL-C ≥ 70 mg/dL) [5]. Veterans with ASCVD are at high risk for recurrent CV events and can benefit greatly in the short and long term from lipid optimization and improved LDL-C management [3,5].
Suboptimal LDL-C management in Veterans with ASCVD has been attributed to various factors including lack of awareness, patient preferences, statin intolerance, clinical inertia, poor adherence to LLTs, and the disagreement on lipid treatment goals and management among care teams and in national guidelines [5,6]. Current VA/Department of Defense (DoD) lipid guidelines suggest that the reduction of LDL-C levels below a threshold 100 mg/dL can prevent the occurrence of CV events, even in high-risk groups [3,7,8]. In contrast, the 2018 American Heart Association (AHA)/American College of Cardiology (ACC) Guideline on the Management of Blood Cholesterol recommends that for high-risk individuals, including those with ASCVD, LDL-C levels be reduced to less than 70 mg/dL for CV event prevention by intensifying statin therapy and using non-statin therapies [3,7,8].
There is a compelling need to address dyslipidemia management, education, and guidelines to improve the cardiovascular health of Veterans with ASCVD and suboptimal LDL-C levels. Quality Improvement (QI) projects play an integral role in the VA Healthcare System; they provide the opportunity to assess barriers to care, identify care solutions, and collaborate with experts, staff, and Veterans to implement sustainable, system wide care improvements. Since a large proportion of Veterans with ASCVD have elevated LDL-C levels, the VA in collaboration with AHA, developed a novel QI program to optimize lipid management for Veterans most at risk of CV events and to reduce CV events and CV-related costs for the VA Healthcare System [5].
The VA Lipid Optimization Reimagined - Quality Improvement (VALOR-QI) program aims to improve clinical pathways and processes that impact the lipid management of Veterans with ASCVD through multifaceted strategies that target four key objectives (Table 1).
| Table 1: Program objectives for VALOR-QI. |
| VALOR-QI Program Objectives |
| Development of an algorithm to identify at-risk Veterans with ASCVD who are suitable for participation in lipid optimization interventions. Assessment of potential barriers to lipid management among Veterans, HCPs treating Veterans with ASCVD, and the VA Healthcare System. Development of a comprehensive assessment of care plans to identify potential barriers to optimizing lipid management for Veterans engaged in the program. Evaluation of the efficacy and long-term safety of various delivery of care models for the management of dyslipidemia, including use of statin and non-statin LLTs, HC interventions, and HCP process and procedure changes. |
| ASCVD indicates Atherosclerotic Cardiovascular Disease; HCPs, Healthcare Providers; VA, Veterans Affairs; LLTs, Lipid Lowering Therapies; and HC, Healthcare Coach. |
Methods
Design
VALOR-QI is an innovative, collaborative three-year multi-site QI program established by the VA and the American Heart Association (AHA). Local VALOR-QI teams at 50 VA Medical Centers (VAMC) will develop and deploy a variety of QI interventions that address site-specific barriers to Veteran lipid optimization.
Participants
VAMC eligibility criteria: A VAMC is eligible for participation in VALOR-QI if it: 1) has an associated Non-Profit Corporation (NPC) to accept funding according to VA third-party funding requirements; 2) has identified a local site lead to serve as Clinical Champion (CC), a Healthcare Coach (HC), and clinical staff to implement the program as the Health Care Provider Network (HCPN); and 3) serves a Veteran population eligible for VALOR-QI that is representative of the diverse nature of US Veterans in factors such as rurality, race, ethnicity, sex assigned at birth, age, social determinants of health, and severity of ASCVD/LDL-C levels (Table 2).
| Table 2: VA Medical Center and Veteran inclusion and exclusion criteria for participation in VALOR-QI. | ||
| VA Medical Center | Veteran | |
| Inclusion Criteria | Has associated NPC CC and HC identified Serves population of eligible Veterans | Age ≥ 18 Diagnosis of ASCVD LDL- C ≥ 70mg/dL or non-HDL- C ≥ 100 mg/dL Seen by member of HCPN member |
| Exclusion Criteria | No ability to receive third-party funding No staff to fulfill critical roles Does not treat populaticon of eligible and diverse Veterans | HCP clinical decision to not engage Veteran Recent CV event that could interfere with acute management |
| NPC indicates Non-Profit Corporation; CC, Clinical Champion; HC, Healthcare Coach; ASCVD, atherosclerotic cardiovascular disease; LDL-C, low density lipoprotein cholesterol; Non-HDL-C, non-high-density lipoprotein cholesterol; HCPN, Health Care Provider Network; HCPs, Healthcare Providers; and CV, cardiovascular. | ||
Veteran eligibility criteria: Veterans must meet the following criteria to be eligible for participation in the VALOR-QI program: 1) over the age of 18 with a history of ASCVD (myocardial infarction, stroke, or peripheral arterial disease); 2) have either LDL-C ≥ 70 mg/dL or non-high-density lipoprotein cholesterol (non-HDL-C) ≥ 100 mg/dL; and 3) be treated by a member of the HCPN. Exclusion criteria for the program include 1) responsible HCP clinical decision to not engage Veteran and 2) Veterans with recent CV events that according to HCP might interfere with acute management (Table 2).
Program structure & activities
The VALOR-QI National Network consists of program oversight provided by the AHA QI Consulting Team and the VA Boston Coordinating Center (BCC), and 50 local site VAMC teams made up of CCs, HCs, a HCPN, and an affiliated NPC (Figure 1).
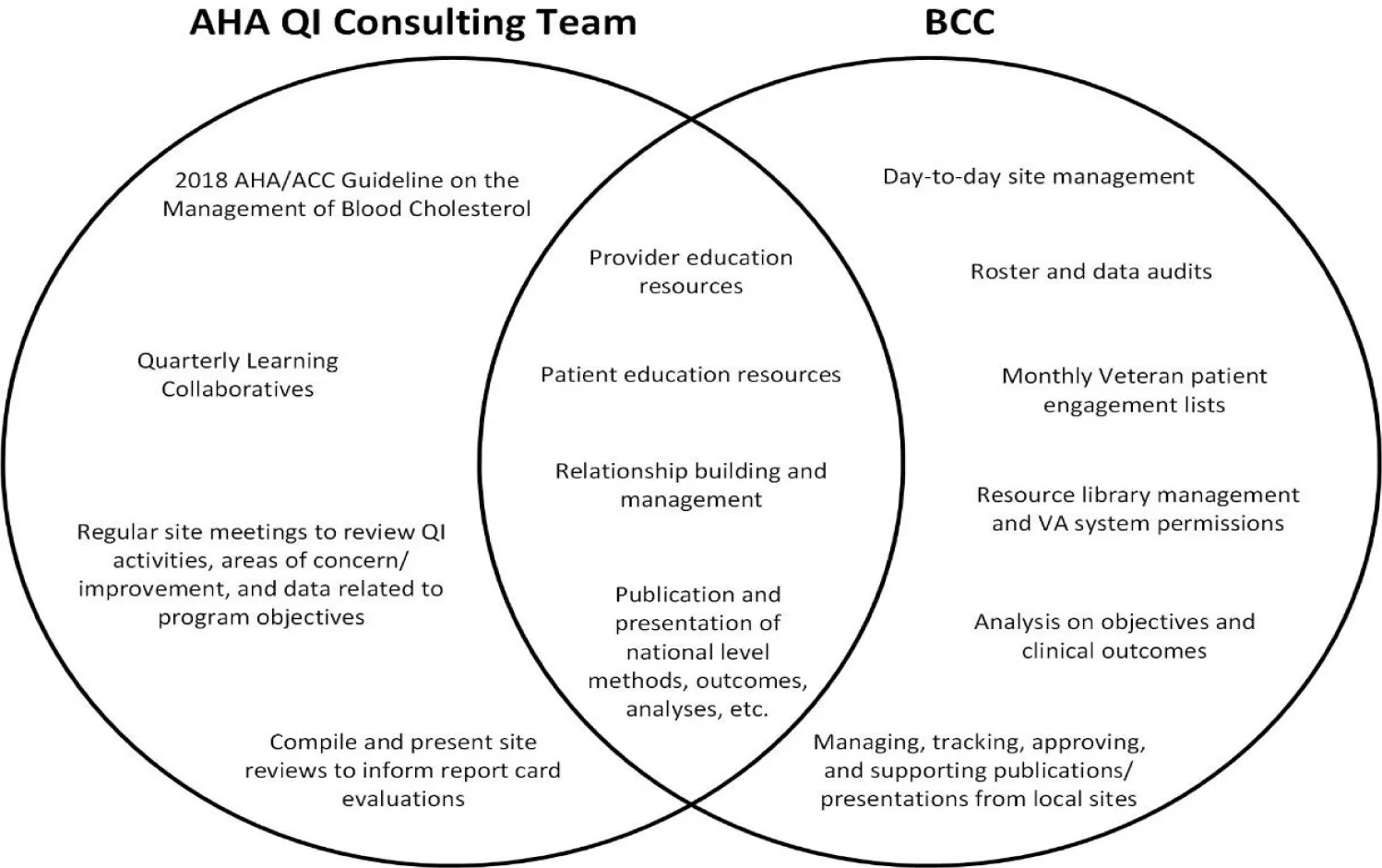
Program oversight: VALOR-QI program administration consists of two entities working together to ensure program goals and objectives are met: the AHA QI Consulting Team and the BCC.
- AHA QI Consulting Team: The AHA brings QI expertise to the program. The VALOR-QI AHA QI Consulting Team consists of four QI consultants who work with assigned sites to assess and document existing lipid management processes, resources, capabilities, and barriers, and develop personalized QI plans to address barriers. The AHA also facilitates quarterly Learning Collaborative calls where participating sites can engage in professional education discussions on lipid management topics and learn strategies and insights from other participating sites.
- Boston Coordinating Center: The BCC is a leader in multi-site VA research, clinical trial, and QI projects. The BCC team provides clinical expertise, unique insight on VA culture and processes, and crucial support in regulatory and contracting activities. The BCC houses VA program leadership, project management, and data management and analysis teams that work with all VALOR-QI sites for the duration of the program.
QI support & facilitation activities: The BCC and AHA teams provide monitoring, support the implementation of QI processes and strategies, and generate program-related resources for participating VALOR-QI sites. Although most program oversight activities span both teams, some roles are unique to each (Figure 2).
- HC support: In close collaboration with the AHA QI Consulting Team, BCC staff provide ongoing support and guidance to HCs as they implement QI interventions at their sites. While supporting activities can vary from site to site, AHA QI Consultants and BCC staff maintain regular and open communication with HCs to check in on progress, troubleshoot challenges, and answer any questions that arise.
- ASCVD algorithms, engagement lists, & monthly metrics: In alignment with VALOR-QI program goals and inclusion/exclusion criteria, the BCC data team deploys algorithms to identify Veterans who may be eligible for the program. Algorithms are applied monthly to produce site-specific Veteran engagement lists and program metric data. These resources are then shared with participating VALOR-QI sites to aid the implementation, monitoring, and ongoing adaptation of their chosen QI strategies.
- Educational & communication materials: AHA and BCC teams develop, compile, and distribute resources for VALOR-QI HCPs, HCs, and Veterans. All materials are housed within the central electronic VALOR-QI Network Resource Library:
- HCPs & HCs: These resources educate providers (including CCs and HCPN team members) and HCs about ASCVD, LLTs, the latest scientific and medical research on reducing the risk of CV events, QI activities and implementation strategies, and best practices for program data entry and monitoring. Communication resources available include provider recruitment letters and VALOR-QI program promotional materials.
- Veterans: A selection of patient-facing educational tools on LLTs, lifestyle interventions, nutrition, and general CV health are available for HCs, CCs, and HCPN team members to share with Veterans engaged in the VALOR-QI program. Veteran communication materials span general program information, templates for Veteran interactions, welcome and check-in letters, and lipid goal achievement certificates.
- AHA QI Consultant Meetings: CCs and HCs are required to attend monthly or bi-monthly meetings with their assigned AHA QI Consultant. These meetings provide opportunities for local site staff to develop and adapt their QI activities, troubleshoot issues and concerns, monitor and analyze their progress, and receive guidance and support from their AHA QI Consultant.
- Learning Collaboratives: Quarterly Learning Collaborative calls are led by the AHA QI Consulting Team and provide a venue for QI model shares presented by sites, educational presentations and discussions on lipid management topics, and breakout sessions for CCs and HCs to share progress and insights.
- Program Database Development & Management: Program data are collected, managed, and audited by the BCC team using Research Electronic Data Capture (REDCap) tools hosted at the VA [9-11]. REDCap is a secure, web-based software platform designed to support data capture, providing 1) an intuitive interface for validated data capture; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for data integration and interoperability with external sources.
- Site Roster and Data Audits: The BCC team conducts quarterly audits of local VALOR-QI site rosters and of VA REDCap data. These audits provide timely monitoring of local site accesses to potentially sensitive information and of required trainings, help to protect Veteran information, maintain the accuracy of HCPN details that inform engagements lists, and ensure the integrity and accuracy of program data entered into the VA RED Cap databases [9-11].
- Brown Bag Lunches, BCC Office Hours, and misc. trainings: Facilitated by the BCC, Brown Bag Lunches are an optional, informal space for local teams to present program-related tips and tricks, foster inter-site collaboration, and to troubleshoot any concerns that arise. The BCC also hosts a monthly Office Hours meeting that allows sites to bring questions to VALOR-QI leadership and to troubleshoot questions or concerns with other sites. Other miscellaneous trainings include review sessions covering VA REDCap [9-11] data entry, VALOR-QI engagement lists, and program status, and are completed on an as needed basis.
VALOR-QI Local Sites: Each participating site includes a CC who is responsible for local site oversight and activities; an HC who is responsible for engaging eligible Veterans and HCPs; an HCPN consisting of providers who treat eligible Veterans and support the implementation of process and procedure changes to optimize lipid management; and an NPC that is responsible for site contracting, staffing, and payments.
- QI Activities: To improve the treatment of dyslipidemia in Veterans with ASCVD, local sites review their unique barriers to lipid management. Barriers are then addressed by implementing a range of QI activities that are generally categorized as direct or indirect based on the level of Veteran engagement (Table 3). These QI activities include, but are not limited to, identifying Veterans with high-risk ASCVD and elevated LDL-C, raising awareness of the importance of LDL-C management, educating Veterans and their providers about cholesterol and ways it can be managed, and providing HC support of Veterans’ lifestyle modifications and use of LLTs. Local sites work with their assigned AHA QI Consultant over the course of the program to review their QI strategies, how well they are working in addressing program objectives, and how to change and adapt QI strategies to meet the ongoing changing needs of their local site.
| Table 3: Direct and Indirect Quality Improvement (QI) Activities Deployed at Local VALOR-QI sites. | ||
| Direct Veteran Engagement Activities | Indirect Veteran Engagement Activities | |
| Definition | QI activities that take place between an HC and Veteran who has been enrolled in the direct cohort of the program. | QI activities that do not include any interaction between an HC and a directly engaged Veteran. Typically, indirect QI strategies include the local site VALOR-QI team addressing clinical processes and procedures. |
| Program Data | Directly engaged Veterans are entered into the VA REDCap database and their activities are collected in VA REDCap for the course of the program. Outcomes are monitored via electronic health record review. | Summary-level data on implementation strategies are documented during AHA QI Consulting Meetings and outcomes are monitored via electronic health record review of eligible Veterans who interact with the local site VALOR-QI team. |
| Examples | In-person meeting between HC and Veteran to discuss lifestyle management goals Phone calls between HC and Veteran to review importance of medication adherence Group classes for HC and Veterans to share lipid management journeys and challenges Notifying Veterans that they have reached LDL-C goals | Establishing a lipid clinic to streamline lipid management at a local VAMC Ordering labs for Veterans who have not had them drawn in over a year Sending HCPN appointment reminders and lipid management recommendations for Veterans with suboptimal LDL-C levels Collaborating with other local VAMC entities such as MOVE!® Weight Management Program, Whole Health, Smoking Cessation, and Pharmacy to leverage local site resources and monitor care plan |
| QI indicates quality improvement; HC: Healthcare Coach; VA: United States Department of Veterans Affairs; VA REDCap, VA Research Electronic Data Capture; AHA, American Heart Association; LDL-C, Low Density Lipoprotein Cholesterol; VAMC, Veterans Affairs Medical Center; and HCPN, Health Care Provider Network. | ||
Outcomes & Program Analysis
Outcomes
The primary clinical outcomes of this program are to increase the percentage of Veterans achieving LDL-C target of less than 70 mg/dL to over 30% and to demonstrate a meaningful change in LDL-C in Veterans with ASCVD not at target LDL-C at baseline.
Secondary outcomes include absolute and percent change in LDL-C, use of LLTs, medication adherence, and healthcare utilization and costs. Lipid optimization outcomes will be evaluated stratified by key Veteran demographics including geographic region, age, assigned sex, race, and ethnicity.
Program analysis
The AHA and BCC teams will develop benchmarks to evaluate program implementation. Metrics will be used to evaluate local- and national-level outcomes at 6 and 12 month intervals. Summary assessment data will be shared with local sites and VALOR-QI leadership on an ongoing basis.
At the completion of the program, analyses will be conducted to determine the overall impact of VALOR-QI on lipid optimization. The BCC will also evaluate cost-effectiveness and healthcare resource utilization associated with the overarching QI program (Table 4).
| Table 4: VALOR-QI data sources and management. | ||||
| Description | Data Collected | Security & Management | Quality Control | |
| VA CDW | Data warehouse that contains electronic health record data for all Veterans receiving care in the VA Healthcare System. | Veteran demographics, LDL-C labs, LLT data, ASCVD and CV disease diagnoses and events, appointments, and healthcare costs and utilization | Data can only be accessed by BCC staff post-training and approval. CDW data are stored on secure VA servers behind the VA firewall. Personnel that are no longer part of the program have their accesses removed immediately upon notification of departure. | CDW’s Data Quality Team ensures data are accurately extracted into the warehouse. Subject matter experts ensure data integration, architecture, and source management. Data quality reviews are conducted daily12 |
| VA REDCap | Secure, web-based database used to enter directly engaged Veterans and their HC interactions. | Veteran identifying information, Veteran demographics, engagement and withdrawal dates, HC interaction dates and types | VA REDCap can only be accessed by BCC and local site staff post-training and approval. Access is limited to the VA server using staff credentials. Personnel that are no longer part of the program have their accesses removed immediately upon notification of departure. | Site entered data are audited on a quarterly basis by the BCC for completeness and accuracy of certain variables. |
| Survey and Consultations | Site-level qualitative and quantitative program data are collected throughout the program via surveys and during consultations. | Quantities of HC activities, adherence to QI activities, changes in clinical processes and procedures, local site satisfaction and feedback, and program sustainability goals | Data from surveys and consultations can only be viewed by BCC and/or AHA QI Consulting Team staff depending on the sensitivity of data collected. Aggregate data are shared with program leadership and sites on an as needed basis. | Survey responses are reviewed for correctness and completeness. Response rates for surveys are monitored and follow up is completed on an as-needed basis to ensure representative site participation. AHA QI consultants document strategies using a tracking document on a quarterly basis. |
| VA indicated United States Department of Veterans Affairs; VA CDW, VA Corporate Data Warehouse; LDL-C, Low Density Lipoprotein Cholesterol; LLT, Lipid Lowering Therapy; ASCVD, Atherosclerotic Cardiovascular Disease; CV, Cardiovascular; BCC, Boston Coordinating Center; VA REDCap, VA Research Electronic Data Capture; HC, Healthcare Coach; QI, Quality Improvement; and AHA, American Heart Association. | ||||
Data collection
Clinical outcome data will be extracted from three main sources: (1) the electronic VA Corporate Data Warehouse (CDW) for indirect Veteran information and all Veteran outcome data, (2) data received from sites via self-report on site QI activities with directly engaged Veterans in VA REDCap databases, and (3) information gathered from VALOR-QI sites during their consultations throughout the program to document insights on local site program activities, experiences, and satisfaction with the VALOR-QI Program (Table 4).
Data management
All Protected Health Information (PHI), Personally Identifiable Information (PII), and sensitive program data are collected and securely stored behind the VA firewall by the BCC and participating sites via VA approved data storage strategies (Table 4). No individual-level data are shared with the AHA, NPCs, or outside of the appropriate local site teams.
Participating sites and BCC team members protect Veteran PHI and PII by encrypting communication with key program entities, implementing access restrictions, and securing paper records. Violations of established data protection measures are documented, reported, and addressed in accordance with VA guidelines.
Quality control
VA REDCap data are audited on a quarterly basis by the BCC. CDW data are reviewed to ensure the accuracy of cohort information, and the codes used to analyze these data are reviewed by a data analyst or epidemiologist with extensive experience working with VA data and trained in code review (Table 4).
Discussion
As both the first ASCVD-focused initiative of its kind and one of the largest known multi-site QI networks in the VA Healthcare System, VALOR-QI presents a critical opportunity for VAMCs to meaningfully impact clinical culture, LDL-C guidelines, and lipid management practices. This initiative aligns with the VA Healthcare System’s commitment to providing Veterans with high quality, holistic, and patient-centered cardiovascular healthcare.
VALOR-QI's dynamic design fosters continuous assessment, adaptation, and refinement of QI strategies deployed at each site, highlighting the program’s unique strengths. By prioritizing flexibility, agility, and sustainability, sites are encouraged to make ongoing adjustments to their local QI plans to address ever-changing barriers and needs. QI strategies are implemented at multiple levels of the VA Healthcare System, and include Veteran-focused healthcare coaching, provider education and trainings, as well as clinical and operational changes. Rich variation in geographic location, VAMC size, Veteran populations served, and staff clinical background among VALOR-QI sites has resulted in a strong network that underscores the considerable breadth and depth of expertise within the VA Healthcare System.
Several areas for overall program improvement have been identified, particularly surrounding site selection and data collection processes. Due to administrative requirements, only those VA locations with a designated NPC were eligible for selection, thus limiting the pool of potentially eligible sites. Program data, self-reported in REDCap and recorded in the VA CDW, are also prone to bias and misclassification. These limitations represent key areas of opportunity for future expansion on this work.
Subsequent VALOR-QI activities include comprehensive outcome analyses that will evaluate the program’s efficacy in optimizing Veteran lipid levels and reducing the economic cost and utilization associated with ASCVD care at VAMCs. Results from these analyses will inform the refinement of best practices for ASCVD management, clinical workflows, Veteran and provider education, and strategies for incorporating lipid-centric health coaching into care models. Ultimately, participating VA leadership, staff, and collaborators are committed to leveraging program findings to sustain and expand upon these impactful activities and initiatives, thereby elevating the standard of care for Veterans with ASCVD within and beyond the VA Healthcare System.
Acknowledgements
We would like to thank the Veterans and all VALOR-QI team members at our 50 participating sites without whom this work would not be possible. We would also like to thank Melissa Young, a subject matter expert from the VA Boston Healthcare System for her contributions to this work and the VALOR-QI Program.
Sources of Funding
The VALOR-QI program is supported by Novartis Pharmaceuticals Corporation.
Disclosures
The contents of this paper do not represent the views of the United States Department of Veterans Affairs or the United States Government. J.M.G received investigator-initiated funding from Novartis for a different ongoing project. Other authors declare that they have no conflict of interest.
References
- Assari S. Veterans and risk of heart disease in the United States: a cohort with 20 years of follow up. Int J Prev Med. 2014 Jun;5(6):703-9. PMID: 25013689; PMCID: PMC4085922.
- Eibner C, Krull H, Brown KM, Cefalu M, Mulcahy AW, Pollard M, Shetty K, Adamson DM, Amaral EF, Armour P, Beleche T, Bogdan O, Hastings J, Kapinos K, Kress A, Mendelsohn J, Ross R, Rutter CM, Weinick RM, Woods D, Hosek SD, Farmer CM. Current and Projected Characteristics and Unique Health Care Needs of the Patient Population Served by the Department of Veterans Affairs. Rand Health Q. 2016 May 9;5(4):13. PMID: 28083423; PMCID: PMC5158228.
- Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019 Jun 18;139(25):e1082-e1143. doi: 10.1161/CIR.0000000000000625. Epub 2018 Nov 10. Erratum in: Circulation. 2019 Jun 18;139(25):e1182-e1186. doi: 10.1161/CIR.0000000000000698. Erratum in: Circulation. 2023 Aug 15;148(7):e5. doi: 10.1161/CIR.0000000000001172. PMID: 30586774; PMCID: PMC7403606.
- Sandesara PB, Virani SS, Fazio S, Shapiro MD. The Forgotten Lipids: Triglycerides, Remnant Cholesterol, and Atherosclerotic Cardiovascular Disease Risk. Endocr Rev. 2019 Apr 1;40(2):537-557. doi: 10.1210/er.2018-00184. PMID: 30312399; PMCID: PMC6416708.
- Virani SS, Akeroyd JM, Smith SC Jr, Al-Mallah M, Maddox TM, Morris PB, Petersen LA, Ballantyne CM, Grundy SM, Stone NJ. Very High-Risk ASCVD and Eligibility for Nonstatin Therapies Based on the 2018 AHA/ACC Cholesterol Guidelines. J Am Coll Cardiol. 2019 Aug 6;74(5):712-714. doi: 10.1016/j.jacc.2019.05.051. PMID: 31370962.
- Virani SS, Akeroyd JM, Nambi V, Heidenreich PA, Morris PB, Nasir K, Michos ED, Bittner VA, Petersen LA, Ballantyne CM. Estimation of Eligibility for Proprotein Convertase Subtilisin/Kexin Type 9 Inhibitors and Associated Costs Based on the FOURIER Trial (Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk): Insights From the Department of Veterans Affairs. Circulation. 2017 Jun 20;135(25):2572-2574. doi: 10.1161/CIRCULATIONAHA.117.028503. Epub 2017 May 2. PMID: 28465286.
- Al Rifai M, Blumenthal RS, Stone NJ, Schofield RS, Orringer CE, Michos ED, Heidenreich PA, Braun L, Birtcher KK, Smith SC, Nambi V, Grundy S, Virani SS. Department of Veterans Affairs (VA) and U.S. Department of Defense (DoD) guidelines for management of dyslipidemia and cardiovascular disease risk reduction: Putting evidence in context. Prog Cardiovasc Dis. 2021 Sep-Oct;68:2-6. doi: 10.1016/j.pcad.2021.08.001. Epub 2021 Aug 8. PMID: 34371083.
- O'Malley PG, Arnold MJ, Kelley C, Spacek L, Buelt A, Natarajan S, Donahue MP, Vagichev E, Ballard-Hernandez J, Logan A, Thomas L, Ritter J, Neubauer BE, Downs JR. Management of Dyslipidemia for Cardiovascular Disease Risk Reduction: Synopsis of the 2020 Updated U.S. Department of Veterans Affairs and U.S. Department of Defense Clinical Practice Guideline. Ann Intern Med. 2020 Nov 17;173(10):822-829. doi: 10.7326/M20-4648. Epub 2020 Sep 22. PMID: 32956597.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009 Apr;42(2):377-81. doi: 10.1016/j.jbi.2008.08.010. Epub 2008 Sep 30. PMID: 18929686; PMCID: PMC2700030.
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O'Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN; REDCap Consortium. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019 Jul;95:103208. doi: 10.1016/j.jbi.2019.103208. Epub 2019 May 9. PMID: 31078660; PMCID: PMC7254481.
- Obeid JS, McGraw CA, Minor BL, Conde JG, Pawluk R, Lin M, Wang J, Banks SR, Hemphill SA, Taylor R, Harris PA. Procurement of shared data instruments for Research Electronic Data Capture (REDCap). J Biomed Inform. 2013 Apr;46(2):259-65. doi: 10.1016/j.jbi.2012.10.006. Epub 2012 Nov 10. PMID: 23149159; PMCID: PMC3600393.
- https://dvagov.sharepoint.com/sites/OITBISL/SitePages/BISL%20Bulletin/Data-Quality-in-the-CDW.aspx
Content Alerts
SignUp to our
Content alerts.
 This work is licensed under a Creative Commons Attribution 4.0 International License.
This work is licensed under a Creative Commons Attribution 4.0 International License.